Ruptured Implant

What should you do when you’ve been told after mammogram or ultrasound that your implant is ruptured?
Surprisingly, this is not all to uncommon of an issue we are seeing in the office on any given day. Breast Augmentation with silicone implants is the number 1 cosmetic surgical procedure worldwide, and performed over 300,000 times a year in the United States. The risk of rupture after 10 years maybe close to 10 percent. Ten percent of 600,000 (300,000 x 2) is 60,000 potential implant ruptures per year. The numbers are staggering and not many plastic surgery teams can invest the time and coordination with breast imagers needed to deal with this complex issue.
Now to be perfectly clear, it isn’t the mammogram itself that causes rupture, so don’t shy away from your routine annual screening that is recommended, but mostly it is degradation of the implant inner and outer shells with the risk of rupture occurring at an increased incidence over time.
It’s very unpredictable to know when an implant shell will rupture, I have seen rupture as early as three years after insertion of the newest fifth generation silicon breast implant, but mostly devices seem to be compromised only after many years following insertion. The severity of the rupture also varies greatly from only internal shell compromise to external shell failure with extrusion of silicon into the surrounding capsular space.
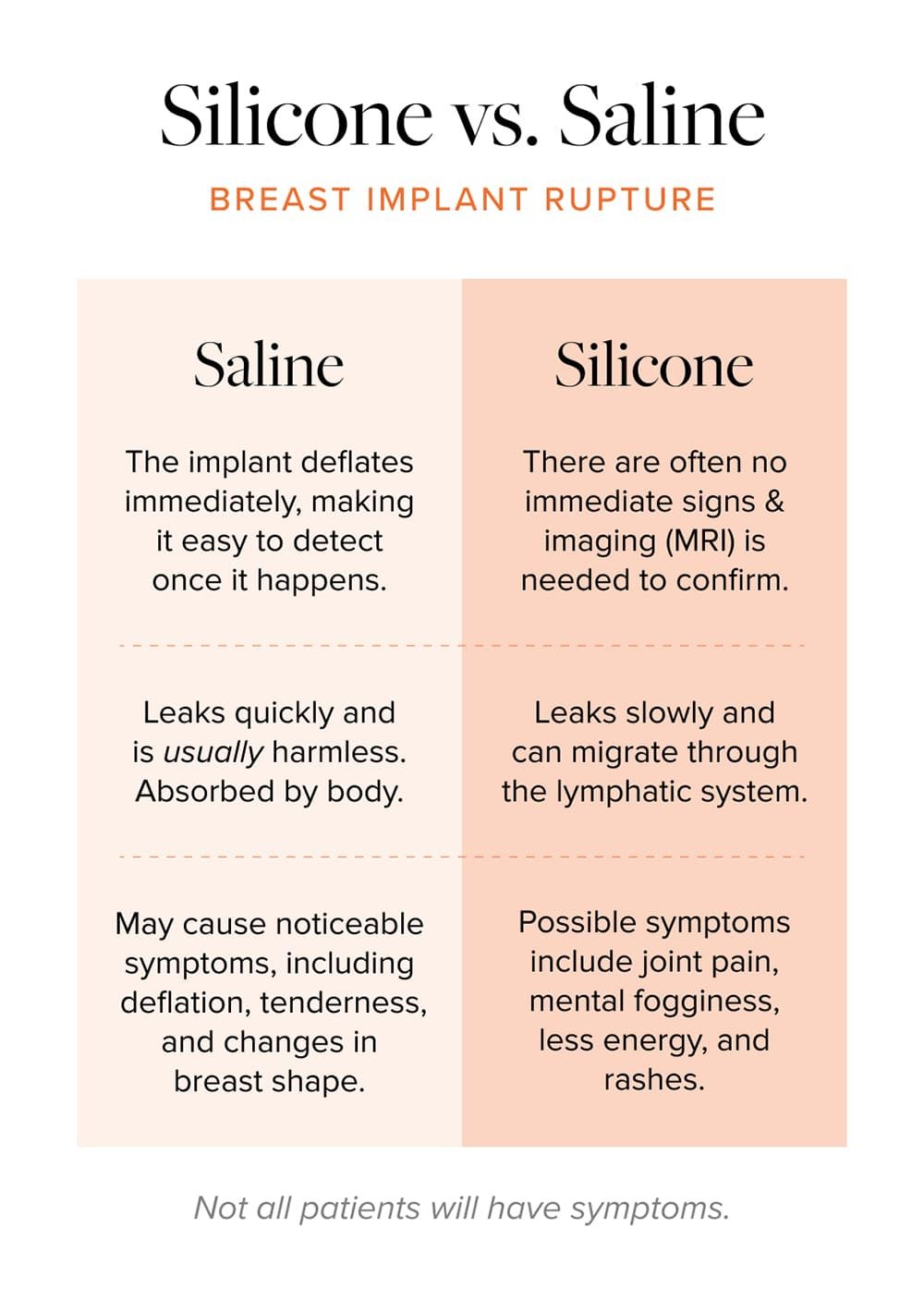
Does it matter if the implant’s internal or external shell is ruptured? Is there risk if this happens? and what are possible signs or symptoms? There are no external signs of rupture for silicone implants unless you have the rare situation of free flowing silicone migrating threw the lymphatic system resulting in enlarged lymph nodes usually under the arm. On the other hand, a saline implant shell rupture would result in immediate deflation and detection. Symptoms of silicone breast rupture may be related to implant related illness such as mental fogginess, joint pain, decreased energy levels, and rashes. Not all patients who have implant rupture will experience breast implant illness like symptoms but it is important to keep in consideration.
If I don’t have any signs of rupture or any symptoms or implant shell failure, should I remove the compromised implant immediately or can I delay intervention?
I think the answer all depends on the severity of rupture determined by imaging and any associated symptoms. It is rare that I see a ruptured implant device that requires immediate removal. Mostly patients with ruptured implants can either maintain the implant due to the limited nature of compromise or have a planned surgery with removal of the compromised device, followed by either reinsertion of implants or reconstruction of the natural breast shape using mammoplasty techniques without the need for implants. If you choose to keep the compromised implant then just make sure you continue to have imaging dedicated to implant evaluation with ultrasound or MRI.
A careful history and physical exam is essential when determining what the next steps should be. Review of all available imaging which may include not only mammogram but also ultrasound and MRI evaluation is also necessary when determining what solution is best.
I have found that in my practice with intracapsular rupture without evidence of external compromise most patients prefer to keep their implant devices. Once, the outer capsule demonstrates failure, then surgical intervention and planning usually follows.
There are many options regarding the surgical treatment of breast implant rupture, but the primary goal is to remove the implant and all silicon that has escaped into the implant pocket. This requires special techniques for insuring as much removal of free silicon as possible with specially designed suction devices and advanced irrigation formulas. I will often combine this with excision of the capsule formed around the implant. After all the silicon has been removed, as well as the implant capsule, then reaping the breast can proceeded. The first step is placing the muscle back into his anatomic position along the chest wall to increase function and strength if the implant was placed under the muscle. After the muscle has been secured then we move onto reshaping the breast using advanced plastic Surgery breast lift patterns (mastopexy). If additional volume is needed, it is often possible to utilize fat grafting of the remaining breast tissue without having to use a new breast implant.
The Recovery following implant removal and revision of the breast is fairly quick and most patients are back to full activity within two weeks.
Breast implant rupture can be extremely stressful once detected, and we are happy to guide you through this difficult decision-making process regarding observation and possible surgical treatment.
Dr K